Every American between the ages of 45-75 should be screened for colon cancer. In the last post we talked about how screening tests are used to check for signs of colon cancer before you have any symptoms. Now we’re going to look at the different types of screening tests and get an idea of which one might be right for you.
What are the different types of screening tests for colon cancer?
Did you know that colon cancer is the third most common cancer in the US? Because it’s so common, a lot of research has been put into catching colon cancer early using screening tests. All this research has led to different ways of finding signs of cancer before it becomes too advanced. The earlier you find and treat cancer, the better your chances of beating it.
There are simple tests that detect blood or cancer DNA in the bowel movements. Radiologists can do special scans to take pictures of the bowels to check for tumors. Some types of tests allow doctors to look directly at the inside of the colon. These tests allow them to see any abnormal areas and take a biopsy at the same time.
Let’s take a closer look at how each of these tests are done, how often they need to be repeated and what information we can get from them.
Stool tests:
Colon cancer is sneaky in its early stages. You might not feel bad. You might not even notice anything different about your bowel movements. But there can be subtle changes that stool tests can pick up.
There are 3 different types of fecal tests that look for changes in your stool.
- Fecal occult blood test (gFOBT): Occult means “hidden” in this case. This test checks for blood in your stool that can’t be seen with the naked eye (and maybe hard to find even with a microscope!) It is one of the oldest tests, but it’s super-easy to do and very inexpensive. The doctor can do it right in the office when you have your annual physical exam. Or they can send you home with a special card and swab. After a bowel movement you just swab your stool and smear it on the filter paper on the card. You seal the card up and send it back to your doctor.
In the doctor’s office, a few drops of a liquid containing a chemical called “guaiac” are placed on the filter. If there is no color change, you simply repeat the test every year. If the filter turns blue, it means blood is in your stool. This doesn’t mean you have cancer, but it does mean you need to find out why there’s blood in your stool. Your doctor will probably recommend that you get a colonoscopy.
It’s important not to take NSAIDs, eat red meat or have citrus/vitamin C for a few days before the test because they can cause a false positive result.
- FIT test: FIT means “fecal immunochemical test.” This test is done pretty much the same way as the gFBOT. Instead of using guaiac, it uses antibodies to look for blood in the stool. FIT test is a more specific test for blood. You don’t have to worry about your medications or what you eat beforehand. If it is abnormal, you will need to follow-up with a colonoscopy right away. FIT test should be done every year.
- FIT-DNA test: FIT-DNA is two tests in one. It checks for hidden blood, just like the FIT test. And it also detects the abnormal DNA of cancer cells. It is different from FIT and gFOBT because you’ll get your kit in the mail. Next, you’ll collect your entire bowel movement in the special container and send it back to the lab.
If any abnormal DNA or blood is found, you’ll need a colonoscopy to make sure there’s no signs of cancer in your colon. FIT-DNA only needs to be done every 3 years if the results are normal.
Radiology test:
A CT colonography or “virtual colonoscopy” is a test done by the radiologist. It uses X-rays and a CT to create a 3-dimensional picture of your colon and rectum. It is a very sensitive test that can detect small abnormalities such as tumors or polyps.
Most people don’t need any sedation for a virtual colonoscopy. The test doesn’t require instruments going into the rectum (it’s non-invasive). But, the colon and rectum have to be cleaned out ahead of time using a “bowel prep.” This means that the day before the scan, you will take some medications that cause your bowels to completely empty out. If stool is still in your colon, it can make it hard for the radiologist to read the scans correctly.
On the day of the test, the radiologist will have you drink “contrast solution” which will help show the lining of the gut on the X-rays. A small tube will be used to place some air into your rectum and colon. Finally, you’ll be asked to hold your breath for a few seconds at a time while the scan is done. You might feel a little bloated for a day or two,until all the air is passed.
A virtual colonoscopy should be done every 5 years if no abnormalities are found. If any area is concerning, you should get a colonoscopy right away.
Direct visualization test (using a camera):
The virtual colonoscopy gives doctors a lot of information, but it can miss some smaller abnormalities. Flexible sigmoidoscopy and colonoscopy are two tests that use cameras to look at the inside of the gut.
Flexible Sigmoidoscopy
Just like with the virtual colonoscopy, you will need to empty your bowels before the procedure. You and your doctor will decide whether you need sedation. Many people don’t want to be sedated. The doctor will have you lie on your side. They’ll lubricate your rectum and insert a small tube. This will allow them to insert some air and a camera. If they see anything abnormal like a polyp, they can go ahead and take a biopsy (cut it out for tests.) A small amount of blood or cramping and bloating can happen after a flexible sigmoidoscopy.
A Flexible sigmoidoscopy only looks at the very last part of the colon and rectum. If you have a tumor or polyp at the beginning of the colon, it won’t be seen. Flexible sigmoidoscopy isn’t usually recommended for screening in the US.
If you and your doctor do decide to go this route, you’ll need to repeat it every five years. If you combine this test with a FIT every year (or FIT-DNA), you’ll only need to do it every 10 years.
Colonoscopy
Although it’s the most complex test, colonoscopy is the gold-standard of screening tests for colon cancer. Colonoscopy requires that you have a full bowel prep the day before. You will need to take medications that cause your bowels to empty completely. A colonoscopy is done by a gastroenterologist (GI doctor). It can be done in a special office, a surgery center or even in the hospital. You will almost always get to go home the same day.
Most people have heavy sedation or go to sleep for this procedure. The doctor will have you lie on your side, lubricate your rectum and insert the tube for the air, camera and biopsy equipment. In a colonoscopy, the doctor looks at the inside of the entire colon from the rectum all the way back to the cecum.
The gastroenterologist will be looking for things like polyps. Polyps are finger-like pieces of tissue that stick out from the lining of the colon. A polyp might not be cancer, but the only way to know for sure is to cut it out and look at it under a microscope. The doctor will also be looking for ulcers, areas of redness or larger masses. If they see anything that doesn’t look normal, they will take a biopsy to make sure that cancer isn’t quietly growing inside you.
The colonoscopy usually doesn’t take more than 60 minutes to do. But you’ll need an hour or two to fully wake up before you can go home. You might have a little bleeding, some cramping or bloating, but you should be back to normal the same day.
If your colonoscopy is normal and you don’t have an increased risk for colon cancer, then you only need to get a colonoscopy every 10 years.
The Bottom Line
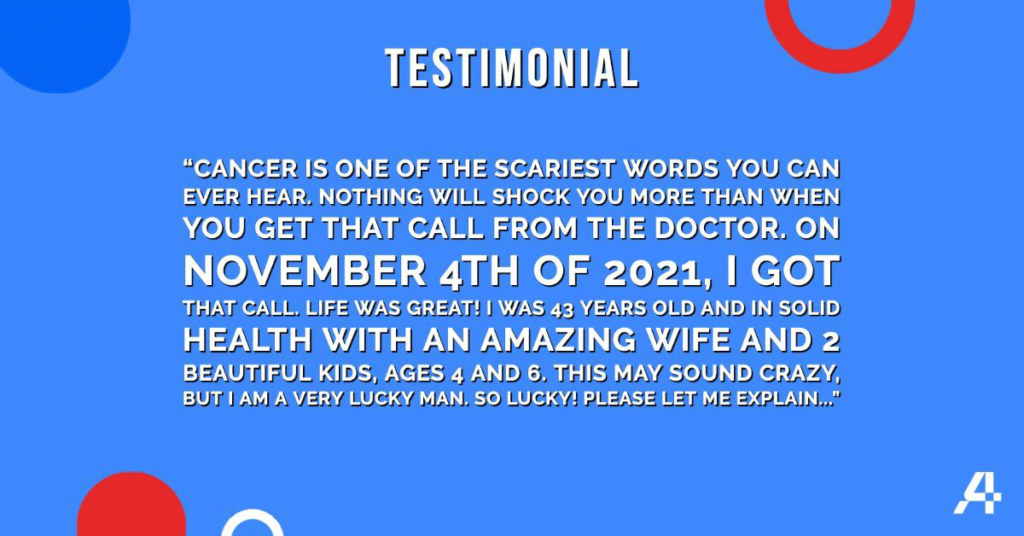
The earlier you catch colon cancer, the more likely you are to beat it. The best way to catch colon cancer early is by doing a screening test on a regular basis, before the cancer gets far enough along to cause symptoms. There are many screening tests available. The best test for you depends on your risk factors and which test you will reliably do on schedule. Get checked starting at age 45. Check it for you. Check it for someone you love. CheckIt4Andretti.
Fast Facts:
- Screening tests check for signs of colon cancer before you have any symptoms
- There are many different screening tests that you can choose from including colonoscopy, stool tests and radiology exams
- The best screening test for you will depend on your risk factors, but it’s also the one you are most likely to do!